Advancing the Understanding of Heart Disease Detection
Providing new insights into the causes and mechanisms underlying heart diseases through original research and published findings.
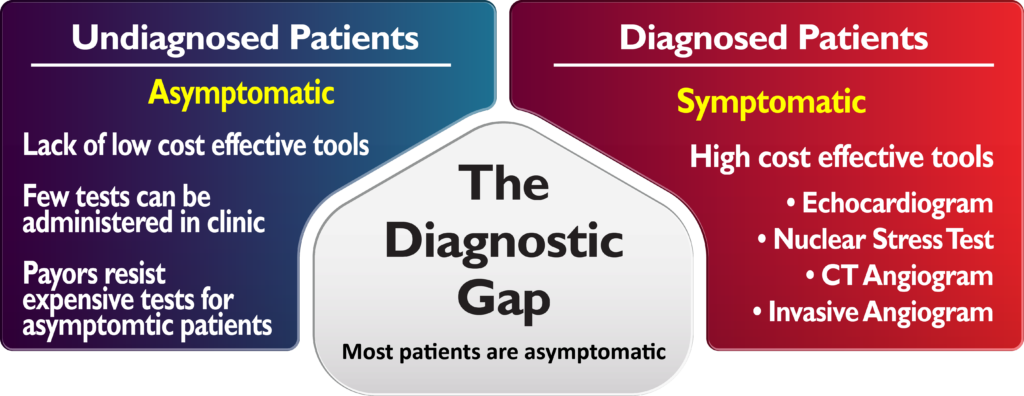
Bridging the Diagnostic Gap in Heart Disease
- Most patients with heart disease are asymptomatic.
- Physicians have limited front-line technology options to detect heart disease.
- Most advanced diagnostic tests are expensive and require referral.
- Payors often discourage advanced diagnostics for asymptomatic patients.
Clinical Publications
Publications Abstract Background Recent guidelines propose N-terminal pro-B-type natriuretic peptide (NT-proBNP) for recognition of asymptomatic left ventricular (LV) dysfunction (Stage B Heart Failure, SBHF) in type 2 diabetes mellitus (T2DM).…
Publications Originally published 29 Dec 2023 https://doi.org/10.1161/JAHA.123. 31671Journal of the American Heart Association. 2024;13:e031671Link to article: Quantitative Prediction of Right Ventricular Size and Function From the ECG | Journal of the…

Publications Joshua Lampert, Akhil Vaid, William Whang, Jacob Koruth, Marc A. Miller, Marie-Noelle Langan, Daniel Musikantow, Mohit Turagam, Abhishek Maan, Iwanari Kawamura, Srinivas Dukkipati, Girish N. Nadkarni, and Vivek Y. Reddy Abstract Background Premature ventricular complexes (PVCs) are prevalent and, although often…
Publications Akhil Vaid, Joy Jiang, Ashwin Sawant, Stamatios Lerakis, Edgar Argulian, Yuri Ahuja, Joshua Lampert, Alexander Charney, Hayit Greenspan, Jagat Narula, Benjamin Glicksberg & Girish N Nadkarni npj Digital Medicine volume 6, Article number: 108 (2023) Link to article: A foundational vision transformer improves diagnostic performance for electrocardiograms…
Reg. US Pat. & TM off.
All Rights Reserved.
Powered by Collective42
HeartSciences’ AI-ECG products are currently in development and not commercially available in the United States.
wavECG and wavEKG are trademarks of HeartSciences.
MV-WBSTE-002 Rev A